The emergence of COVID-19 vaccines has generated immense excitement, but the supply chain in Australia now face the complex task of securing and distributing supplies to Australians and administrating the vaccine. Acquiring sufficient quantities is just the start; the vaccines must then be transported safely to multiple destinations, maintained at the right temperature, and tracked at all times to avoid tampering and assure product integrity and delivery.
Here are three ways that can optimize the vaccine supply chain in Australia:
1) Planning is the key to success
An effective supply chain puts the vaccine receiver at its heart, and aims for speedy execution with minimum wastage, at an agreed and understood cost-to-serve. It should make the most of existing distribution and cold storage capabilities (for flu jabs or other vaccines) and offer the potential to scale up if necessary.
Good planning is necessary to understand the capacity of infrastructure and critical assets (e.g. refrigerated trucks, fridges at GPs/family practices) to be able to deliver effectively. Demand planning comes to the fore when millions of doses of vaccine are required. Those responsible for procurement must swiftly evaluate different manufacturers of vaccines, syringes and refrigeration equipment, determined in part by their location, capacity, and compliance with licensing and other regulatory requirements. With several vaccines available — and more possibly in the pipeline — there is the option to use multiple manufacturers.
While this can increase volume, it also adds to the complexity, as different products may require different storage conditions and have varying expiry dates. Complexity is further increased as over the coming months, governments and health systems will be transporting COVID-19 vaccines to hundreds and possibly thousands of destinations — at a level far beyond current vaccine distribution. They need to assess the available transportation options, check whether airports and ports can handle the increased traffic, and map the many routes.
One major decision is whether to coordinate centrally or adopt a more devolved or more hybrid model based on the patient and location (metro, regional, remote) differentiation. Given the high demand for the vaccine, it may not be possible to ramp up the existing estate of suitable vehicles with cold storage and fragile stock facilities.
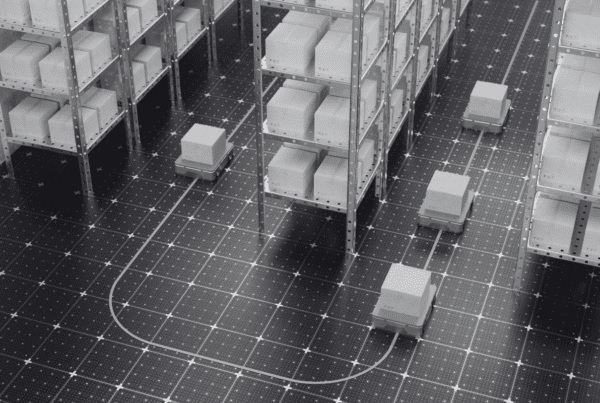
Third-party logistics companies are likely to fill the gap, with the option of one or more providers for national, regional and/or local deliveries. The procurement or logistics team could also consider appointing a lead provider to coordinate other providers. Despite the high priority of vaccines, there should be models for the costs of transport at different frequencies of delivery, to make the most cost-effective choice. These providers must practice robust inventory management, to optimize product flows from suppliers and wholesalers, supported by strict controls over temperature and handling throughout the product journey.
2) Track and trace
Complete, end-to-end inventory visibility is vital, to understand when vaccines will be available for use, and to avoid damage or theft. Data on tags from COVID-19 vaccine batches enable efficient tracking, giving supply chain managers a complete picture of the volumes stored or in transit, as well as any vaccines, delivered but not yet used. Stock can also be identified according to the manufacturer and expiry date — which is important, given the relatively short shelf life. All of which enables better demand planning, to inform decisions on ordering, distribution, order allocation, storage and returns, optimizing product flows and avoiding overload and wastage.
Track and trace calls for a robust data analytics capability, and an established process for capturing, storing, transferring and processing real-time data. In such a large and complex supply chain, involving multiple players and geographies, one should not underestimate the importance of taxonomies and common language. Asset data standardization agreed taxonomies, and commercial data sharing can all help to generate common understanding, visibility and compliance.
3) Manage last-mile delivery, returns and post-vaccine tracking
Last-mile delivery is one of the most critical parts of the COVID-19 vaccine supply chain in Australia. The number and location of vaccination sites will be determined by the percentage of the population to be vaccinated, the priority groups, the population density, availability of trained frontline workers, and the distance the target population must travel to access health facilities. Longer-distance journeys of bulk vaccine freight are typically made by larger trucks, with smaller trucks and carriers taking over for the ‘last-mile’, performing multiple drops to healthcare centres, pharmacies and hospitals.
Accurate volume flow is critical to avoid wastage: even the larger distribution points can only accept 5–7 days of stock due to on-site capacity limitations and cold chain requirements. The last-mile delivery vehicles must be equipped with cold chain storage and precious cargo facilities, commandeered by licensed drivers, and integrated into track and trace systems to assure 24/7 visibility for both delivery and returns (due to expired stock, overstocking, or damaged stock). Ideally, one truck or carrier should manage both outbound fulfilment and returns, offering transport, processing, storage and destruction. They will be responsible for the integrity of returns and show there has been no replacement or theft of vaccines.
The Australian government and healthcare systems are accustomed to distributing vaccines to different segments of the population. But the COVID-19 vaccine is of a different magnitude; not just in terms of scale, but in its huge potential impact on the world’s health, social and economic wellbeing. That’s why it’s so important to achieve a fast, efficient and responsive supply chain, bringing together the best of public and private capabilities, demonstrating best practice at every stage.